 David Zweig wrote in the Atlantic Our Most Reliable Pandemic Number Is Losing Meaning. Excerpts in italics with my bolds.
David Zweig wrote in the Atlantic Our Most Reliable Pandemic Number Is Losing Meaning. Excerpts in italics with my bolds.
From the start, COVID hospitalizations have served as a vital metric for tracking the risks posed by the disease. Last winter, this magazine described it as “the most reliable pandemic number,” while Vox quoted the cardiologist Eric Topol as saying that it’s “the best indicator of where we are.” On the one hand, death counts offer finality, but they’re a lagging signal and don’t account for people who suffered from significant illness but survived. Case counts, on the other hand, depend on which and how many people happen to get tested. Presumably, hospitalization numbers provide a more stable and reliable gauge of the pandemic’s true toll, in terms of severe disease. But a new, nationwide study of hospitalization records, released as a preprint today (and not yet formally peer reviewed), suggests that the meaning of this gauge can easily be misinterpreted—and that it has been shifting over time.
If you want to make sense of the number of COVID hospitalizations at any given time, you need to know how sick each patient actually is. Until now, that’s been almost impossible to suss out. The federal government requires hospitals to report every patient who tests positive for COVID, yet the overall tallies of COVID hospitalizations, made available on various state and federal dashboards and widely reported on by the media, do not differentiate based on severity of illness. Some patients need extensive medical intervention, such as getting intubated. Others require supplemental oxygen or administration of the steroid dexamethasone. But there are many COVID patients in the hospital with fairly mild symptoms, too, who have been admitted for further observation on account of their comorbidities, or because they reported feeling short of breath. Another portion of the patients in this tally are in the hospital for something unrelated to COVID, and discovered that they were infected only because they were tested upon admission. How many patients fall into each category has been a topic of much speculation. In August, researchers from Harvard Medical School, Tufts Medical Center, and the Veterans Affairs Healthcare System decided to find out.
The study found that from March 2020 through early January 2021—before vaccination was widespread, and before the Delta variant had arrived—the proportion of patients with mild or asymptomatic disease was 36 percent. From mid-January through the end of June 2021, however, that number rose to 48 percent.
In other words, the study suggests that roughly half of all the hospitalized patients showing up on COVID-data dashboards in 2021 may have been admitted for another reason entirely, or had only a mild presentation of disease.
One of the important implications of the study, these experts say, is that the introduction of vaccines strongly correlates with a greater share of COVID hospital patients having mild or asymptomatic disease. “It’s underreported how well the vaccine makes your life better, how much less sick you are likely to be, and less sick even if hospitalized,” Snyder said. “That’s the gem in this study.”
But the study also demonstrates that hospitalization rates for COVID, as cited by journalists and policy makers, can be misleading, if not considered carefully. Clearly many patients right now are seriously ill. We also know that overcrowding of hospitals by COVID patients with even mild illness can have negative implications for patients in need of other care. At the same time, this study suggests that COVID hospitalization tallies can’t be taken as a simple measure of the prevalence of severe or even moderate disease, because they might inflate the true numbers by a factor of two. “As we look to shift from cases to hospitalizations as a metric to drive policy and assess level of risk to a community or state or country,” Doron told me, referring to decisions about school closures, business restrictions, mask requirements, and so on, “we should refine the definition of hospitalization. Those patients who are there with rather than from COVID don’t belong in the metric.”
Another Problem: Can Hospitals Covid Numbers Be Trusted?

Gateway Pundit published a pertinent article Missouri COVID Whistleblower: Hospitals are Lying to the public about COVID… and I can prove it. Excerpts in italics with my bolds.
Josh Snider worked in facilities management at Missouri Baptist Medical Center or “MBMC”, “I watched our hospital administrators say in the media that our intensive care units were overflowing with COVID patients, at 98% capacity, knowing that it was a complete and utter lie.”
Snider relates that the MBMC hospital, part of a larger $5.5 billion annual network within the Barnes Jewish hospital system in St. Louis, Missouri, actually shut down three out of four floors of intensive care during COVID because they were UNUSED.
“And even after shutting down three-fourths of our ICU capacity, they were still never more than 50% full with that drastically reduced overall capacity. These medical systems that are saying they are overrun with COVID patients are likely LYING TO THE PUBLIC,” Snider said.
Snider provided documentary proof of the COVID case load of the MBMC system, whose COVID patients do not track national trends, and where the number of COVID patients in ICU were, at many points, a single, solitary person.
“I would have to adjust the airflow in some of the rooms of people in the ICU with COVID, they were fine. I believe in COVID, I know it’s serious, but I also personally saw people who were fine, they had a terminal case of boredom. I spoke with these people and they weren’t sick at all, they felt fine but were told they had to stay there. Many brought their PlayStations with them to waste away the days with video games instead.”

This chart was INTERNAL and distributed to employees of MBMC. In it, you can see that the number of COVID patients in critical care was always under 20. The hospital shut down 3 of 4 ICU wings, and in the remaining one had the capacity for 60 beds/patients. They never came close to being at capacity for COVID ICU patients.
These charts, provided by Snider, show that there was a relatively normal track for COVID infections at the MBMC Center, an acute care facility in St. Louis. Even during periods of infection spikes in the national population, those spikes are not found in the hospital data. As well, the bottom line showing serious cases of COVID requiring intensive care remain significantly small and reduced throughout the months of the pandemic.
Here is the chart generated from information submitted to the US Department of Health and Human Services, as published by the Gannett News Service:
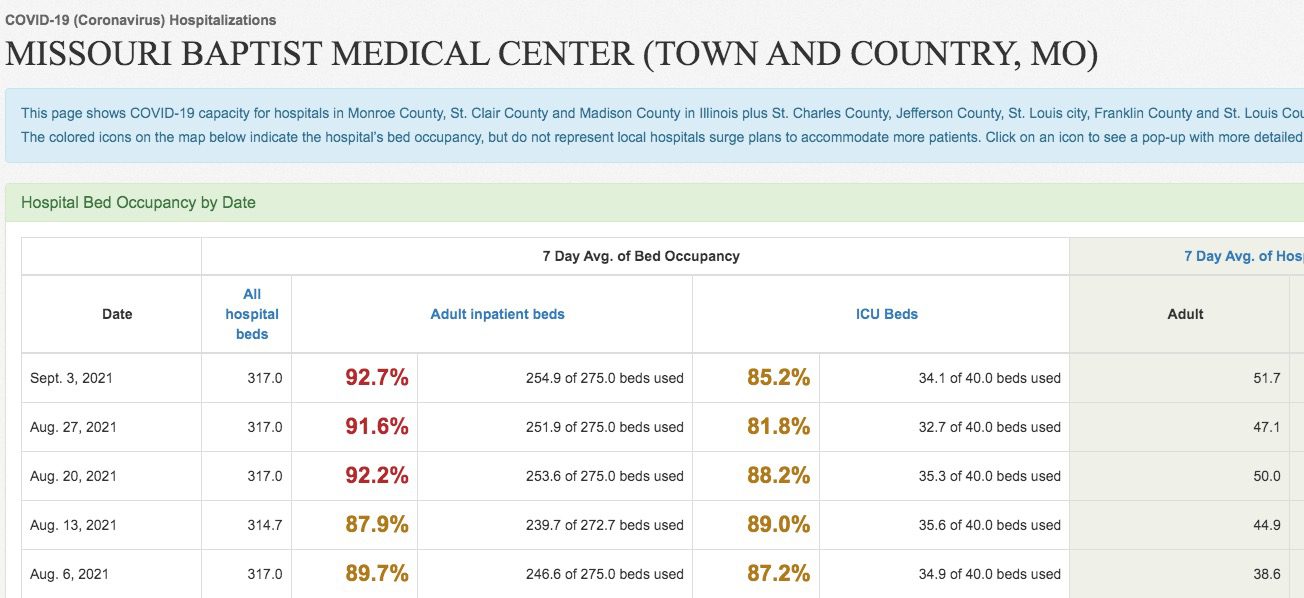
INTERNAL: on August 18, 2021, MBMC said they had 19 COVID patients in ICU.
EXTERNAL: on August 20, 2021, MBMC told the public they had 35.3 COVID patients in ICU.
THE PUBLIC NUMBERS ARE OFF FROM THE INTERNAL REPORTS OF COVID PATIENTS IN THE ICU BY ALMOST 100%
Snider has provided his personal statement, documentary evidence, and clear data discrepancies that all suggest that hospitals are not telling the public the truth about the COVID pandemic.
“The real flu season in the hospital was always more serious than COVID has been,” Snider said. “Flu season in a hospital is very challenging, and even the tamest flu season in years past was still worse than COVID has been so far. The people who have been suffering and sadly dying are clearly people who are hundreds of pounds overweight, and people with multiple other comorbidities like stage 4 cancer. I’m not a Doctor, but the response and panic to this virus is clearly wildly disproportionate to reality.”
LikeLike
really nice article
LikeLike
peter, not sure how your comment relates to covid hospital numbers?
LikeLike