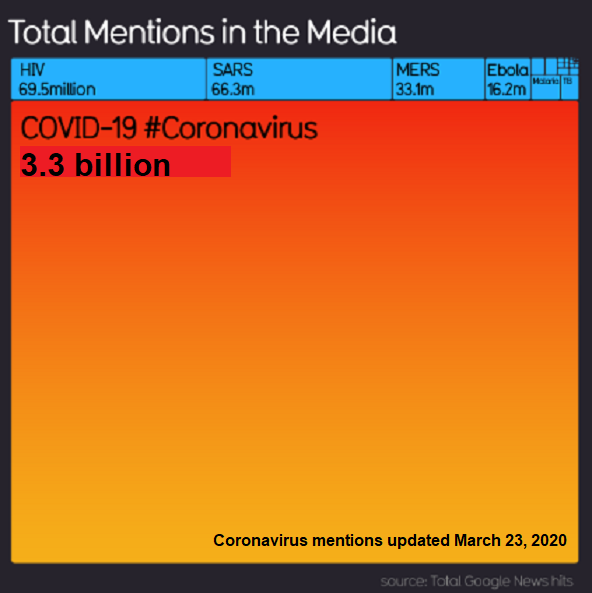
Media Blowing on Embers of Covid Fear
Alex Berenson explains in a twitter thread (here). Text in italics with my bolds
1/ This panic is likely to prove even more embarrassing than previous panics. Here’s why: the media is both confused and conflating several different data points in an effort to stir hysteria. (Stop me if you’ve heard this before.)
What do I mean?
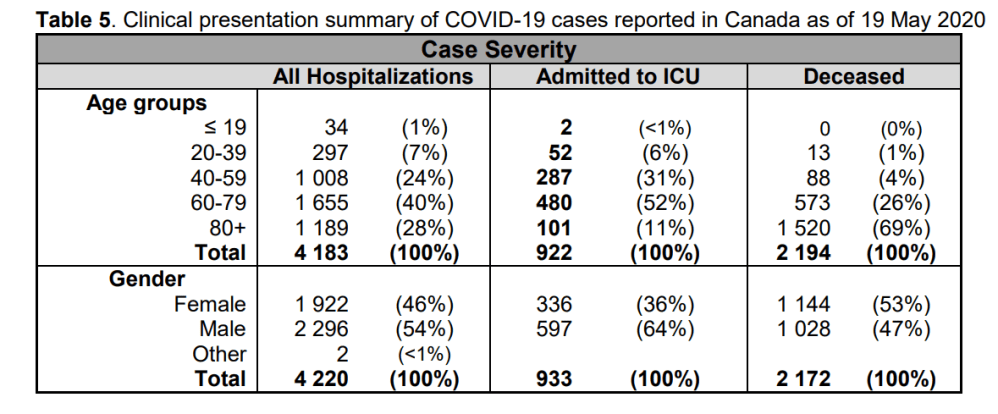
2/ So: you’ve heard positive tests are up in several states. True. The media refers to these as “cases,” as if positive tests have clinical significance by themselves. They do not. The vast majority of people with positive tests do not become ill enough to need hospitalization…
3/ Much less intensive care or ventilator support. For people under 50, this is true in the extreme. But the daily age distribution of positive tests is rarely if ever supported…
4/ Second: you’ve heard overall hospitalizations are up in some states. This is also true. THIS IS A FEATURE, NOT A BUG. Overall hospitalizations are rising because people are returning to hospitals for elective (and in some cases very necessary) surgeries that were postponed…
5/ Now, in some of these states COVID-related hospitalizations have also risen (though they make up a tiny fraction of overall hospitalizations). Scary, right?
No. When people go to the hospital for elective surgeries they are now routinely tested for COVID...
6/ Whether or not they are symptomatic. Hospitals have financial and legal as well as medical incentives to do this. IF THEY ARE POSITIVE, hospitals will report them as COVID patients (since, technically, they are), EVEN IF THEY HAVE NO COVID SYMPTOMS.
7/ This fact accounts for the bizarre disconnect between the fact the number of people going to emergency rooms with influenza-like or COVID-like symptoms is NOT rising (and remains in the low single digits) even in states reporting more hospitalizations…
8/ As well as the fact that fewer hospitalized cases are now progressing to ventilators (I can’t swear to this in every state, but it appears to be a trend)…
9/ And the fact that deaths no longer seem to have any relationship to case counts in many states (true even accounting for the fact that deaths lag).
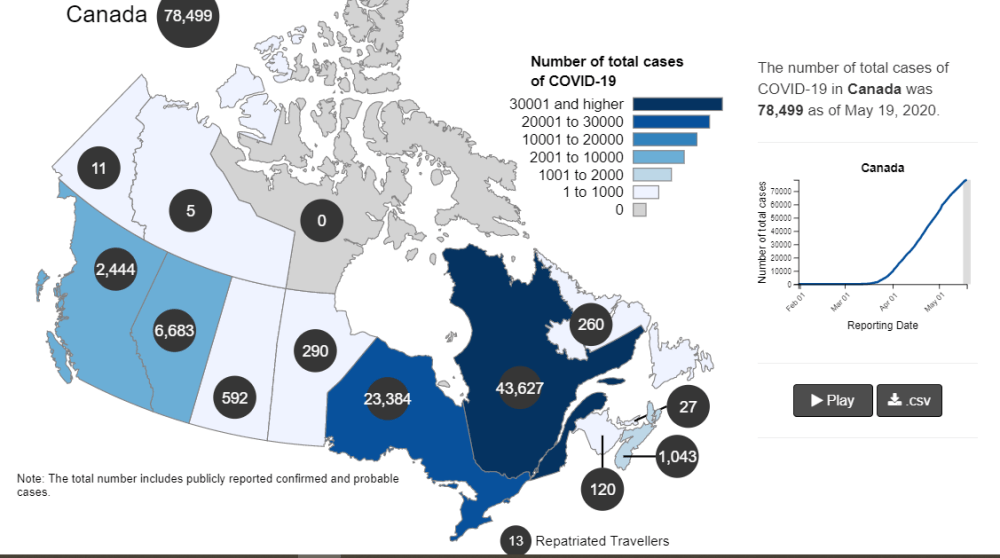
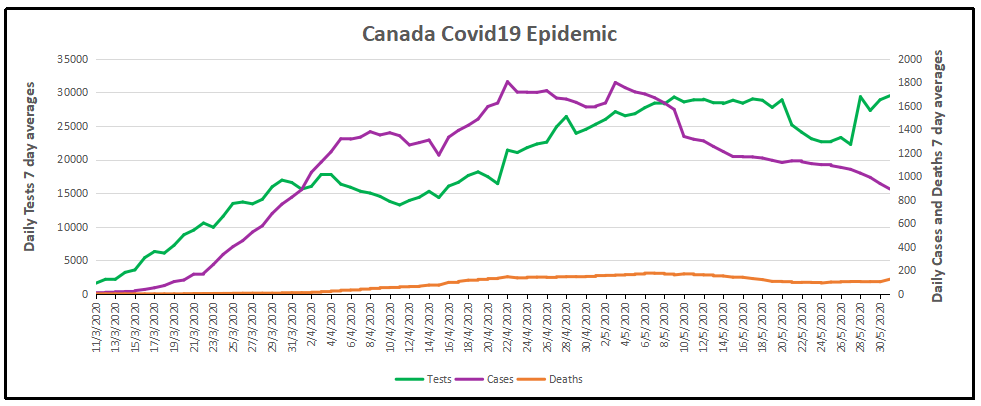
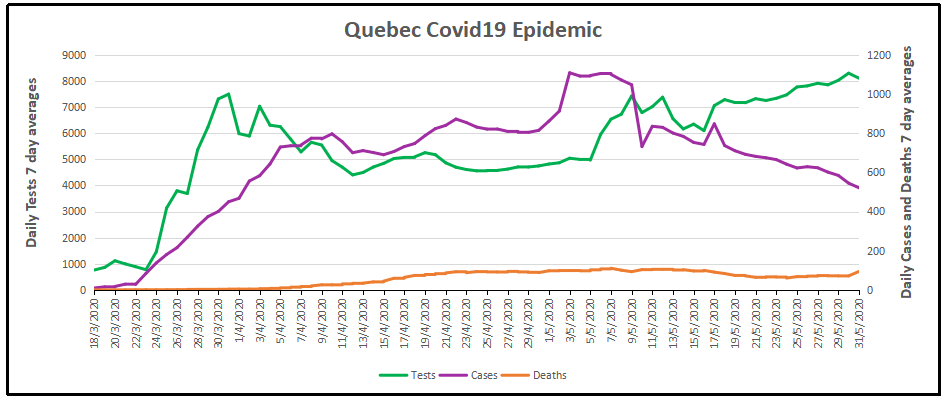
The question you should be asking yourself: why aren’t Europe and Asia seeing post-lockdown spikes if this trend is real?
10/ And don’t say masks. Masks are not routine in Europe. So either COVID is somehow different post-lockdown in Europe (and different in different states, too)… or this is just one last gasp of panic porn.
And if you want confirmation from epidemiologists, here Facts about Covid-19 from Swiss Policy Research.
Fully referenced facts about Covid-19, provided by experts in the field, to help our readers make a realistic risk assessment. (Regular updates below)
“The only means to fight the plague is honesty.” (Albert Camus, 1947)
Overview
1.According to the latest immunological and serological studies, the overall lethality of Covid-19 (IFR) is about 0.1% and thus in the range of a strong seasonal influenza (flu).
2. Even in global “hotspots”, the risk of death for the general population of school and working age is typically in the range of a daily car ride to work. The risk was initially overestimated because many people with only mild or no symptoms were not taken into account.
3. Up to 80% of all test-positive persons remain symptom-free. Even among 70-79 year olds, about 60% remain symptom-free. Over 95% of all persons develop at most moderate symptoms.
4. Up to 60% of all persons may already have a certain cellular background immunity to Covid19 due to contact with previous coronaviruses (i.e. common cold viruses).
5. The median or average age of the deceased in most countries (including Italy) is over 80 years and only about 4% of the deceased had no serious preconditions. The age and risk profile of deaths thus essentially corresponds to normal mortality.
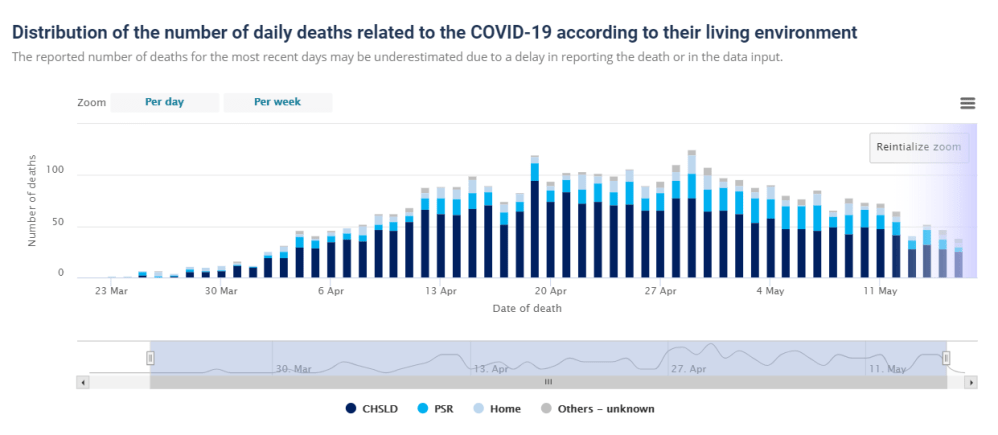
6. In many countries, up to two thirds of all extra deaths occurred in nursing homes, which do not benefit from a general lockdown. Moreover, in many cases it is not clear whether these people really died from Covid19 or from weeks of extreme stress and isolation.
7. Up to 30% of all additional deaths may have been caused not by Covid19, but by the effects of the lockdown, panic and fear. For example, the treatment of heart attacks and strokes decreased by up to 60% because many patients no longer dared to go to hospital.
8. Even in so-called “Covid19 deaths” it is often not clear whether they died from or with coronavirus (i.e. from underlying diseases) or if they were counted as “presumed cases” and not tested at all. However, official figures usually do not reflect this distinction.
9. Many media reports of young and healthy people dying from Covid19 turned out to be false: many of these young people either did not die from Covid19, they had already been seriously ill (e.g. from undiagnosed leukaemia), or they were in fact 109 instead of 9 years old. The claimed increase in Kawasaki disease in children also turned out to be false.
10. The normal overall mortality per day is about 8000 people in the US, about 2600 in Germany and about 1800 in Italy. Influenza mortality per season is up to 80,000 in the US and up to 25,000 in Germany and Italy. In several countries Covid19 deaths remained below strong flu seasons.
11. Regional increases in mortality can occur if there is a collapse in the care of the elderly and sick as a result of infection or panic, or if there are additional risk factors such as severe air pollution. Special regulations for dealing with the deceased sometimes led to additional bottlenecks in funeral or cremation services.
12. In countries such as Italy and Spain, and to some extent the UK and the US, hospital overloads due to strong flu waves are not unusual. In addition, up to 15% of doctors and health workers are now being put into quarantine, even if they develop no symptoms.
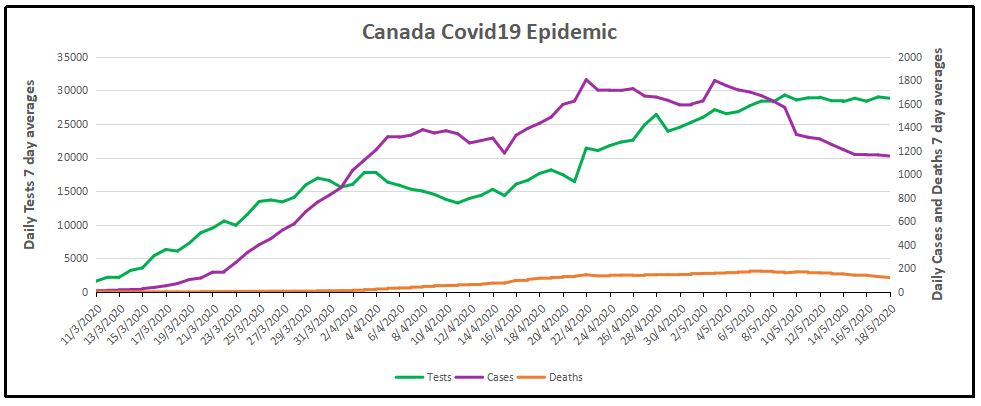
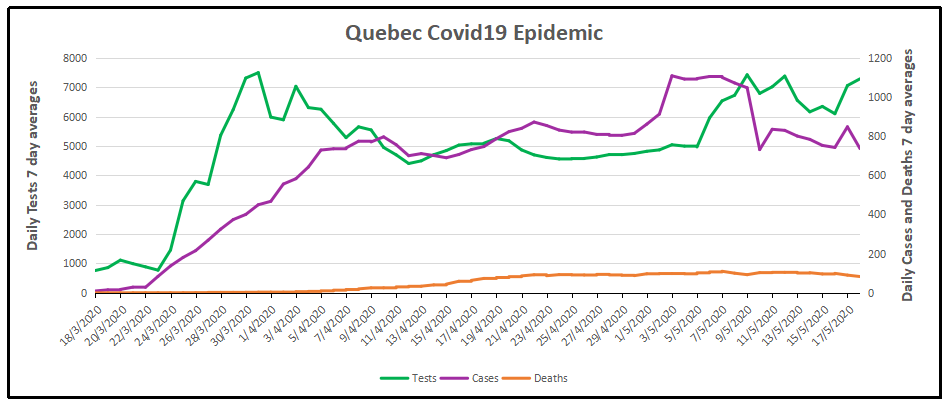
13. The often shown exponential curves of “corona cases” are misleading, as the number of tests also increased exponentially. In most countries, the ratio of positive tests to tests overall (i.e. the positive rate) remained constant at 5% to 25% or increased only slightly. In many countries, the peak of the spread was already reached well before the lockdown.
14. Countries without curfews and contact bans, such as Japan, South Korea or Sweden, have not experienced a more negative course of events than other countries. Sweden was even praised by the WHO and now benefits from higher immunity compared to lockdown countries.
15. The fear of a shortage of ventilators was unjustified. According to lung specialists, the invasive ventilation (intubation) of Covid19 patients, which is partly done out of fear of spreading the virus, is in fact often counterproductive and damaging to the lungs.
16. Contrary to original assumptions, various studies have shown that there is no evidence of the virus spreading through aerosols (i.e. tiny particles floating in the air) or through smear infections (e.g. on door handles or smartphones). The main modes of transmission are direct contact and droplets produced when coughing or sneezing.
17. There is also no scientific evidence for the effectiveness of face masks in healthy or asymptomatic individuals. On the contrary, experts warn that such masks interfere with normal breathing and may become “germ carriers”. Leading doctors called them a “media hype” and “ridiculous”.
18. Many clinics in Europe and the US remained strongly underutilized or almost empty during the Covid19 peak and in some cases had to send staff home. Numerous operations and therapies were cancelled, including many cancer screenings and organ transplants.
19. Several media were caught trying to dramatize the situation in hospitals, sometimes even with manipulative images and videos. In general, the unprofessional reporting of many media maximized fear and panic in the population.
20. The virus test kits used internationally are prone to errors and can produce false positive and false negative results. Moreover, the official virus test was not clinically validated due to time pressure and may sometimes react positive to other coronaviruses.
21. Numerous internationally renowned experts in the fields of virology, immunology and epidemiology consider the measures taken to be counterproductive and recommend rapid natural immunisation of the general population and protection of risk groups.
22. At no time was there a medical reason for the closure of schools, as children hardly ever transmit the virus or fall ill with it themselves. There is also no medical reason for small classes, masks or ‘social distancing’ rules in schools.
23. The claim that only severe Covid-19 but not influenza may cause venous thrombosis and pulmonary (lung) embolism is not true, as it has been known for 50 years that severe influenza greatly increases the risk of thrombosis and embolism, too.
24. Several medical experts described vaccines against coronaviruses as unnecessary or even dangerous. Indeed, the vaccine against the so-called swine flu of 2009, for example, led to sometimes severe neurological damage and lawsuits in the millions.
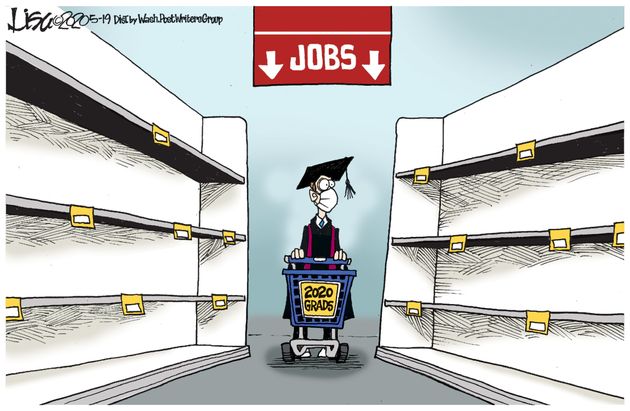
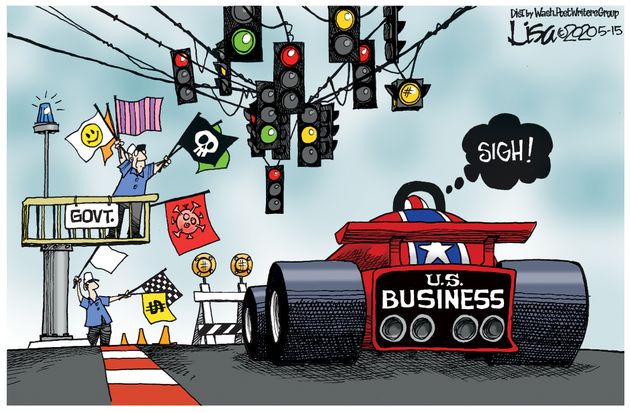
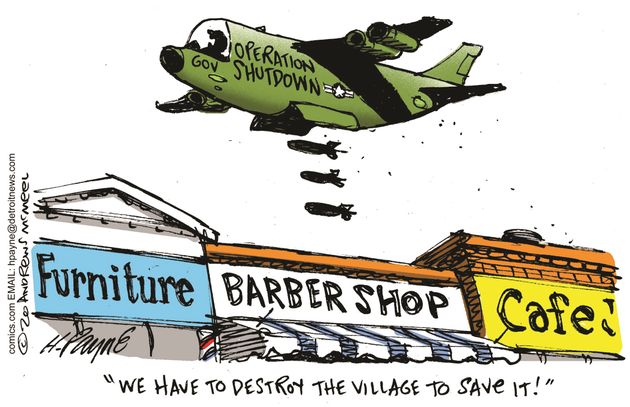
25. The number of people suffering from unemployment, depressions and domestic violence as a result of the measures has reached historic record values. Several experts predict that the measures will claim more lives than the virus itself. According to the UN millions of people around the world may fall into absolute poverty and famine.
26. NSA whistleblower Edward Snowden warned that the “corona crisis” will be used for the massive and permanent expansion of global surveillance. The renowned virologist Pablo Goldschmidt spoke of a “global media terror” and “totalitarian measures”. Leading British virologist professor John Oxford spoke of a “media epidemic”.
27. More than 500 scientists have warned of an “unprecedented surveillance of society” through problematic apps for “contact tracing”. In some countries, such “contact tracing” is already carried out directly by the secret service. In several parts of the world, the population is already being monitored by drones and facing serious police overreach.
28. A 2019 WHO study on public health measures against pandemic influenza found that from a medical perspective, “contact tracing” is “not recommended in any circumstances.

See also: Pandemonia Funnies Madebyjimbob












 Beyond including people with the virus who clearly didn’t die from it, the numbers are inflated by counting people who don’t even have the virus. New York has classified many cases as coronavirus deaths even when postmortem tests have been negative. The diagnosis can be based on symptoms, even though the symptoms are often similar to those of the seasonal flu.
Beyond including people with the virus who clearly didn’t die from it, the numbers are inflated by counting people who don’t even have the virus. New York has classified many cases as coronavirus deaths even when postmortem tests have been negative. The diagnosis can be based on symptoms, even though the symptoms are often similar to those of the seasonal flu.

 One of the things we learned in organizational science was that managers are prone to focus attention and resources on urgent situations at the expense of more serious threats to viability. Thus the aphorism: “When you are up to your ass in alligators it’s difficult to remember that your initial objective was to drain the swamp”. Many times we consultants saw clients working hard to put out fires (complaints, delays, etc.) while oblivious to strategic weaknesses eroding their ability to compete with rivals. One memorable client responded to our product profitabilty analysis showing why they were losing money, “I can’t drop that product, it’s our best seller!”
One of the things we learned in organizational science was that managers are prone to focus attention and resources on urgent situations at the expense of more serious threats to viability. Thus the aphorism: “When you are up to your ass in alligators it’s difficult to remember that your initial objective was to drain the swamp”. Many times we consultants saw clients working hard to put out fires (complaints, delays, etc.) while oblivious to strategic weaknesses eroding their ability to compete with rivals. One memorable client responded to our product profitabilty analysis showing why they were losing money, “I can’t drop that product, it’s our best seller!”